Facial Paralysis
Twitching, weakness or paralysis of the face is a symptom of some disorder involving the facial nerve. A facial nerve disorder may be caused by many different diseases, including infection, injury (trauma), blood flow disturbances, or tumor.
Function/Anatomy of the Facial Nerve
There are two facial nerves, one on each side of our face; the right nerve moves the right side of our face and the left moves the left side of our face. The facial nerve resembles a telephone cable and contains hundreds of individual nerve fibers. Each fiber carries electrical impulses to a specific facial muscle. Acting as a unit, the facial nerve allows us to laugh, cry, smile or frown; hence the name “the nerve of facial expression.” Each of the two facial nerves not only carry nerve impulses to the muscles of one side of the face, but also carry nerve impulses to the tear glands, salivary glands in the mouth, to the muscle of a small middle ear bone (stapes) and transmit taste fibers from the front of the tongue and pain fibers from the ear canal. As such, a disorder of the facial nerve may result in:• twitching, weakness or paralysis of the face
• dryness of the eye and/or of the mouth
• loss of taste
• increased sensitivity to loud sounds in the ear on the side of the paralysis
• pain in the ear on the side of the paralysis
The facial nerve starts at the base of the brain and then travels through a narrow tunnel in the bone surrounding the ear (temporal bone). In one part of the temporal bone, the facial nerve travels alongside the nerves for hearing and balance. Along its inch-and-a-half course through a small bony canal in the temporal bone, the facial nerve is located near the three middle ear bones, in back of the eardrum, and then through the bone behind the outer ear (the mastoid bone) to exit below the ear. Once outside the mastoid bone, the facial nerve divides into many branches (see Figure below) to cause the facial muscles to move.
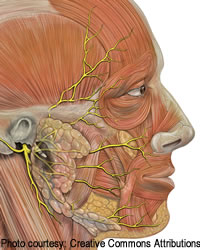
Anatomic view of the facial nerve showing the five main branches of the face (yellow lines are the facial nerve branches).
Diagnosis of Facial Nerve Disorders
A facial nerve disorder may be caused by infection, injury (trauma), blood flow disturbances, or tumor. Testing is often necessary to determine the cause of the disorder and the prognosis for recovery of normal facial movement. These tests may include:• Hearing Test: Performed to determine if the hearing mechanism has been involved.
• Imaging (Radiological) Studies: An MRI and/or CT scan may be performed if the paralysis is due to trauma, or if a stroke or tumor is suspected.
• Tests of facial nerve electrical function [Electroneuronography (ENoG) and electromyography (EMG)]: These tests are very important tools to determine if surgery is necessary in cases of Bell’s palsy or trauma when there is complete facial paralysis. ENoG and EMG helped to determine the prognosis for return of facial function.
Injury/Trauma of the Facial Nerve
The most common cause of facial nerve injury is skull fracture. Motor vehicle accidents are a common cause of facial paralysis from a skull fracture. Hearing loss and balance problems are common symptoms that accompany the symptom of facial paralysis from skull fracture.Operations on the ear may also cause an injury to the facial nerve. Facial paralysis after ear surgery, fortunately, is very uncommon. Facial paralysis may occur, however, when the facial nerve is not in its normal anatomical position (congenital abnormality), or when the nerve is so distorted by the mastoid or middle ear disease that it is not identifiable. In rare cases, it may be necessary to remove a portion of the nerve in order to eradicate the surrounding disease.
Treatment of an Injured Facial Nerve
Medical treatment of a traumatized facial nerve is warranted when the nerve is considered to be intact (i.e. not cut) and not severely damaged by swelling or compression. Medical treatment is the same as described for Bell’s palsy.Surgical Treatment is indicated when the nerve has been cut or when the facial nerve has been severely damaged by swelling or compression. When the nerve has been cut, the nerve can be grafted (reconnected) using a nerve for skin sensation found in the neck. Total paralysis will be present until the nerve regrows through the graft. This usually takes 4 to 15 months. Some facial nerve weakness usually remains for years.
When the facial nerve has been damaged by swelling or compression, the pressure on the nerve can be reduced through surgical decompression of the bone surrounding the nerve.
Acoustic Tumor
The most common tumor to involve the facial nerve is a nonmalignant fibroid tumor of the hearing and balance nerve called an acoustic neuroma. Although there is rarely any weakness of the face before surgery, tumor removal sometimes results in weakness or paralysis. This weakness usually subsides in three months without treatment.It may be necessary to remove a portion of the facial nerve in order to remove the acoustic tumor. In that case the face is totally paralyzed until the nerve is repaired and has had a chance to regrow. It may be possible to sew the nerve ends together at the time of surgery or to insert a nerve graft. At times the nerve anastomosis procedure is necessary, connecting the tongue or shoulder nerve to the facial nerve.
Facial Nerve Neuroma
A nonmalignant fibroid growth may grow in the facial nerve itself, producing a gradually progressive facial nerve paralysis. Removal of this facial nerve neuroma requires severing the facial nerve. Usually it is possible to graft it at the time with a skin sensation nerve from the neck. Total paralysis will be present until the nerve regrows through the graft, usually a period of 4 to 15 months. Some facial weakness usually remains for years.Removal of a facial nerve neuroma may necessitate removal of the inner ear structures. If this were necessary, it would result in a total loss of hearing in the operated ear and temporary severe dizziness.
Mastoid Infection
Acute or chronic middle ear infections occasionally cause a weakness of the face due to swelling or direct pressure on the nerve. In acute infections the weakness usually subsides as the infection is controlled and the swelling around the nerve subsides.Facial nerve weakness occurring in chronically infected ears is usually due to pressure from a cholesteatoma (skin-lined cyst). Mastoid surgery is performed to eradicate the infection and relieve nerve pressure.
Hemifacial Spasm
Hemifacial spasm is an uncommon disease of unknown cause which results in spasmodic contractions of one side of the face. Extensive investigation is necessary at times to establish the diagnosis correctly. Facial nerve decompression (see Bell’s palsy) may be beneficial.Brain Disease
Tumors and circulatory disturbances of the nervous system may cause facial nerve paralysis. The most common example of this is a stroke. Treatment of facial paralysis due to brain disease is managed by an internist, neurologist or neurosurgeon.Eye Care
The most serious complication that may develop as a result of complete facial nerve paralysis is an ulcer of the cornea of the eye. It is most important that the eye on the involved side be protected form this complication. Closing the eye with the finger is an effective way of keeping the eye moist. One should use the back of the finger rather than the tip in doing this to ensure that the eye is not injured.The following are recommendations for eye care in cases of facial paralysis:
• The eye should be covered when outside to prevent particles from becoming lodged in the eye. Glasses or a clear eye bubble may be used to cover the eye.
• Artificial tears are used to keep the eye moist.
• Eye ointment (e.g. Lacrilube) is recommended prior to sleeping in cases of severe/total paralysis
A gold weight inserted into the eyelid is an additional way of protecting the eye in some cases of long-standing paralysis. The gold weight helps the eye to close through gravity.